|
Abstract Giant visceral aneurysms (or pseudoaneurysms) are aneurysmal lesions of the splanchnic vessels that are larger than 5 cm in diameter. As with other visceral aneurysms, treatment may be either surgical or endovascular. Both treatments face challenges given the anatomical complexity of such lesions. However, in the era of novel tools and techniques that have been developed in this field, an increasing number of giant visceral aneurysms can now be treated using endovascular approaches. The purpose of this article is to offer an overview of the most current techniques and trends in the endovascular treatment of giant visceral artery aneurysms. Keywords: Visceral artery aneurysms, endovascular treatment, coils, covered stents, embolisation, surgery Disclosure: MEK is on the Vascular & Endovascular Review editorial board; this did not influence peer review. All other authors have no conflicts of interest to declare. Received: Accepted: Published online: Correspondence Details: Miltiadis Krokidis, School of Medicine, National and Kapodistrian University of Athens, 1st Department of Radiology, Areteion Hospital, 76 Vas Sophias Ave, 11528, Athens, Greece. E: mkrokidis@med.uoa.gr Open Access: This work is open access under the CC-BY-NC 4.0 License which allows users to copy, redistribute and make derivative works for non-commercial purposes, provided the original work is cited correctly.
|
Visceral artery aneurysms (VAAs) are a quite rare but potentially life-threatening vascular disorder involving predominantly the splenic and the common hepatic arteries and less frequently the coeliac, left gastric or branches of the superior mesenteric arteries. The incidence is between 1% and 2% in the general population and splenic artery aneurisms represent approximately two-thirds of them.1–4 VAAs are usually detected and treated when they reach a threshold diameter of 2 cm. Very rarely they may silently grow and reach a size larger than 5 cm. In such cases, they are referred to as ‘giant’ VAAs (GVAAs).5–7 GVAAs may be discovered as an incidental finding on a scan, or they may cause compression symptoms – mainly to the stomach – or present as a rupture.8–10 Because of the risk of rupture, surgical or endovascular treatment is required imminently when such lesions are discovered.
Management of Giant Visceral Artery Aneurysms
Surgical repair has historically been the treatment of choice for all visceral aneurysms.11,12 However, a less invasive endovascular approach has also been gradually adopted in a number of centres – in line with local expertise and available tools – and is now the first option in most centres.13–21 Both surgical and endovascular approaches present challenges in the treatment of these lesions and these are described in more detail in the following sections.
Surgery
Most commonly, GVAAs originate from the splenic artery. Giant aneurysms originating from the hepatic artery or the coeliac trunk are much less common and carry a higher element of complexity when surgical repair is attempted.6,22 For giant aneurysms of the splenic artery, aneurysmectomy with or without splenectomy is expected to be more feasible for lesions located in the proximal or the distal third of the vessel.23,24 For giant splenic artery aneurysms located in the mid portion of the artery, therefore attached to the pancreas, simple ligation of the proximal and distal segments of the artery might be the preferred strategy. Aneurysm ligation without vascular reconstruction is also the preferred option in acute settings for haemodynamically unstable patients. For hepatic GVAAs, aneurysmectomy with vessel reconstruction is required for lesions that are located distally to the origin of the gastroduodenal artery whereas simple ligation may be performed for proximal lesions because of the presence of the collateral circuit.25 Coeliac giant aneurysms are extremely rare and most of them are diagnosed in post mortem examinations – in part because these lesions can also be infectious.26 Surgical approaches also include aneurysmorrhaphy and revascularisation with vein or prosthetic grafts. If the aneurysm includes trifurcation, complexity is significantly increased and mortality reaches 5%.27
Surgical access might be obtained with standard laparotomy – mainly for splenic giant aneurysms.28 This would comprise a left subcostal approach, dissection of the greater omentum with ligatures up to the omental sac followed by dissection and clamping of the two ends of the splenic artery and aneurysmectomy. For coeliac lesions, access might be more challenging. The coeliac trunk may not be accessible anteriorly because of the large size of the mass and a thoracoabdominal incision with retroperitoneal access to the vessels through the gastrocolic ligament might be required.24 Another similar approach might be performed with a chevron incision and rotation of the viscera medially.25 Sometimes control of the artery may be difficult to achieve and additional manoeuvres might be necessary such as medial rotation of the upper abdominal viscera to gain retroperitoneal access to the abdominal aorta. Laparoscopic approaches may also be used as an alternative given the lower morbidity, although there is very limited experience for the treatment of GVAAs.29,30
In cases where arterial reconstruction that would preserve flow towards the organs distally to the aneurysm is not possible, additional visceral resection may be required.31 Surgical options include splenectomy or even distal pancreatectomy when necessary.32,33 Multi-step procedures and combined treatment (both endovascular and surgical) may also be considered in complicated cases and successful use of this approach in the management of a patient with multiple GVAAs has been reported.34
Although data on the surgical management of GVAAs are limited, it is reasonable to assume that morbidity and mortality would increase proportionally for larger lesions. On the other hand – given the dramatic improvement in endovascular techniques and materials – endovascular approaches may also be feasible for challenging cases with unfavourable anatomy and complex sac morphology and are now considered as the first treatment option.
Endovascular Management
The endovascular approach is associated with early postoperative recovery and consequently shorter hospital stays. It represents a valid alternative in high-risk patients with multiple comorbidities and those with a history of abdominal surgery for whom intraperitoneal adhesions may be a concern.
An essential prerequisite in planning endovascular treatment is the availability of good quality, high-resolution imaging. This should include dynamic CT scans and multi-planar reconstructions in order to assess vascular anatomy of the district and determine the most appropriate treatment strategy.
When dealing with GVAAs, endovascular management may be more challenging and many operators are concerned about potential complications and long-term outcomes. Moreover, scientific literature is lacking in studies concerning the management of GVAAs and only a few case reports have been described.35–39
Spiliopoulos et al. advocated the efficacy of endovascular treatment in larger size aneurysms.40 They reported a high clinical and technical success rate dealing with VAAs with a mean diameter of 49.4 ± 21 mm and visceral artery pseudoaneurysms (VAPAs) with a mean diameter of 25.1 ± 14.6 mm. Procedural technical success was achieved in all cases. The target lesion re-intervention rate was 6.1% (2/33 cases) in the VAPA group and 14.2% (3/21) in the VAA group.
A recent systematic review by Hamid et al. analysed 92 cases of giant splenic artery aneurysm.41 Endovascular treatment was considered successful in 89.7% of patients (35/39). The researchers compared endovascular and surgical treatments and noted a comparable efficiency in the reduction of aneurysm-related death and palliation of aneurysm-related symptoms. The study also revealed a higher rate of post-procedure complications with endovascular treatment (p<0.05). However, this outcome may be subject to further interpretation. In fact, in the scenario of splenic artery GVAAs, embolisation of the feeding vessels is often strictly related to the possible onset of splenic infarcts and it can be considered as a minimum loss compared with the risk of splenectomy. So, the authors agreed that endovascular therapeutic techniques – even in the scenario of GVAAs – may be associated with a lower rate of major complications.41
Considerations for Endovascular Techniques
Endovascular management of GVAAs is challenging and requires a combination of several techniques and materials from the interventional armamentarium, including coils, vascular plugs, liquid embolic agents and covered stents. Moreover, the procedure can be performed in a multistage fashion, in order to occlude the several efferent vessels progressively and reduce radiation exposure to the patient.42 The strategy may represent a risk due to the dynamic flow and pressure change inside the sac that may lead to a sudden rupture.
Length of the neck, tortuosity of the arteries, the precise location of the aneurysm and angulation of the aneurysmal tract should be evaluated carefully prior to deciding the embolisation device and technique. It should also be taken into account that a combination of several treatment techniques might be necessary in most cases.
The double inflow-outflow blockage technique is of paramount importance in order to diminish the risk of reperfusion. All the efferent vessels that originate from the sac – usually multiple in giant aneurysms – need to be embolised in order to obtain a complete exclusion of lesion. The outflow vessels should be addressed first.
Selective micro-catheterisation of small arteries originating from huge sacs is a rather challenging task and, in some cases, partial embolisation of the aneurysmal sac helps in reducing the flow and visualising all the feeding vessels. In these cases, the use of liquid embolic agents is very useful as they may reach distal vessels.35
The endovascular coiling approach has been demonstrated to be effective even in very large aneurysms, and more than sufficiently fast and safe to use in the event of a ruptured visceral aneurysm and a sudden drop in blood pressure.36
The packing technique, to prevent the risk of endoleaks, due to the large space in the sac, may be performed using different embolic agents such as fragments of guidewire, long detachable coils (only recently available for peripheral interventions) or liquid agents in order to obtain a better thrombosis of the aneurysm. However, isolated sac packing has been reported to be associated with a high risk of coil compaction and recanalisation of the aneurysmatic sac.19 In fact, in partially thrombosed aneurysms, even sufficient packing does not preclude recanalisation of the aneurysm because factors other than compaction, such as thrombus resolution and migration of coils into the thrombus, cause the aneurysm to recanalise over time. Therefore, in giant-sized aneurysms, the presence or not of sac thrombus may be of paramount importance, as sufficient coil packing to prevent revascularisation would result in significant additional cost, time, and radiation exposure to the patient with equivocal overall benefit.35,36,42–44 In order to achieve a better post-coiling result, the use of the combination of liquid embolics, such as ethylene vinyl alcohol copolymer (Onyx), with coil has been reported with good results.37
The use of covered stents, although virtually appealing for preserving the vessel patency as reported in the literature, is not feasible in most cases for dealing with GVAAs because of the absence of an optimal landing zone, significant tortuosity and evidence of an infected sac.19,38
Even the use of some interesting techniques derived from the endovascular neurointervention experience has been applied in the case of GVAAs. For example, Gjoreski et al. reported a case of GVAA of the hepatic artery successfully treated with dual-layer stents placement as a flow-diverting option.39
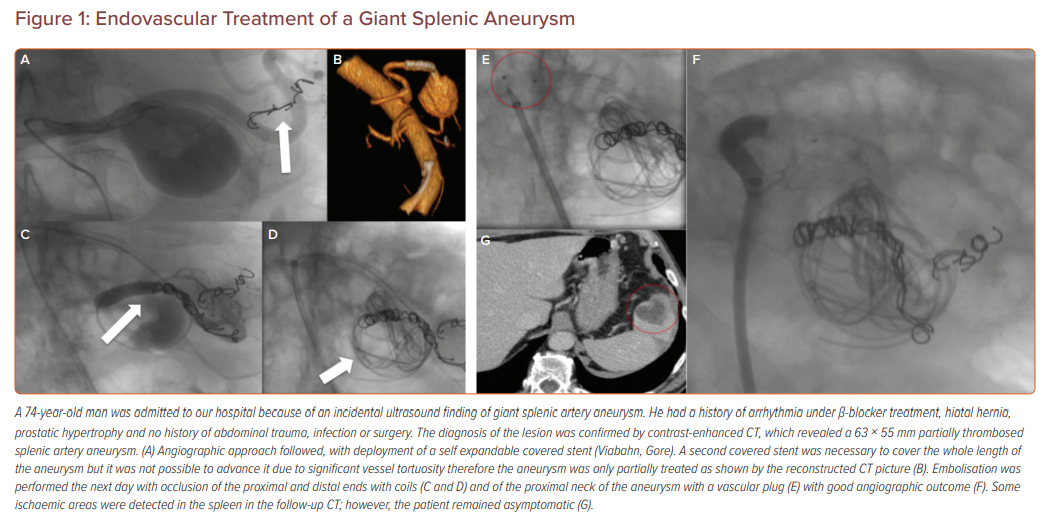
Figure 1 describes the management of a patient in our hospital after the incidental ultrasound discovery of a giant splenic artery aneurysm.
Conclusion
In summary, the management of GVAAs is a complex issue that has to be carried out in very experienced centres. Preliminary studies available in the literature suggest that endovascular treatment is efficient and safe and may be considered as the first-line approach thanks to the low associated morbidity and mortality. However, when considering endovascular exclusion for GVAAs of the abdominal cavity, it is recommended that the patient is haemodynamically stable, there are no signs of aneurysm rupture, there is an experienced team of interventional radiologists and the surgical team is aware and on-board in case of complications or acute rupture. Further studies are necessary to assess the efficacy of this technique in the treatment of haemodynamically unstable patients due to the rupture of the sac.
References
- Hossian A, Reis ED, Dave SP et al. Visceral artery aneurysms: experience in a tertiary-care center. Am Surg 2001;67:432–7.
PubMed - Pasha SF, Gloviczki P, Stanson AW et al. Splanchnic artery aneurysms. Mayo Clinic Proc 2007;82:472–9.
Crossref| PubMed - Shanley CJ, Shah NL, Messina LM. Common splanchnic artery aneurysms. Ann Vasc Surg 1996;10:315–22.
Crossref| PubMed - Chiesa R, Astore D, Guzzo G, et al. Visceral artery aneurysms. Ann Vasc Surg 2005;19:42–8.
Crossref| PubMed - Kim JH, Rha SE, Chun HJ et al. Giant aneurysm of the common hepatic artery: US and CT imaging findings. Abdom Imaging 2010;35: 212–4.
Crossref| PubMed - Bachar GN, Belenky A, Lubovsky L, et al. Sonographic diagnosis of a giant aneurysm of the common hepatic artery. J Clin Ultrasound 2002;30:300–2.
Crossref| PubMed - Yadav S, Sharma P, Singh PK, et al. Giant splenic artery aneurysm: a rare but potentally catastrophic surgical challenge. Int J Surg Case Rep 2012;3:533–6.
Crossref| PubMed - Kemal Beksac and Derya Karakoc. Multiple giant splenic artery aneurysms causing sinistral (left-sided) portal hypertension. Case Rep Gastrointest Med 2016;2016:6278452.
Crossref| PubMed - Debnath J, George RA, Rao PP, Ghosh K. Splenic artery aneurysm–a rare cause for extrahepatic portal venous obstruction: a case report. Int J Surg 2007;5:351–2.
Crossref| PubMed - Elamurugan TP, Kumar SS, Muthukumarassamy R, Kate V. Splenic artery aneurysm presenting as extrahepatic portal vein obstruction: a case report. Case Rep Gastrointest Med 2011;2011:908529.
Crossref| PubMed - Pulli R, Dorigo W, Troisi N et al. Surgical treatment of visceral artery aneurysms: a 25-year experience. J Vasc Surg 2008;48:334–42.
Crossref| PubMed - Marone EM, Mascia D, Kahlberg A et al. Is open repair still the gold standard in visceral artery aneurysm management? Ann Vasc Surg 2011;25:936–46.
Crossref| PubMed - Tulsyan N, Kashyap VS, Greenberg RK, et al. The endovascular management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg 2007;45: 276–83.
Crossref| PubMed - Belli AM, Markose G, Morgan R. The role of interventional radiology in the management of abdominal visceral artery aneurysms. Cardiovasc Intervent Radiol 2012;35:234–43.
Crossref| PubMed - Shukla AJ, Eid R, Fish L, et al. Contemporary outcomes of intact and ruptured visceral artery aneurysms. J Vasc Surg 2015;61:1442–8.
Crossref| PubMed - Laganà D, Carrafiello G, Mangini M, et al. Multimodal approach to endovascular treatment of visceral artery aneurysms with stent-graft: technique and long term follow-up. Cardiovasc Intervent Radiol 2008;31:36–42.
Crossref| PubMed - Balderi A, Antonetti A, Ferro L, et al. Endovascular treatment of visceral artery aneurysms and pseudoaneurysms: our experience. Radiol Med 2012;117:815–30.
Crossref| PubMed - Loffroy R, Favelier S, Pottecher P, et al. Endovascular management of visceral artery aneurysms: when to watch, when to intervene? World J Radiol 2015;7:143–8.
Crossref| PubMed - Cappucci M, Zarco F, Orgera G, et al. Endovascular treatment of visceral artery aneurysms and pseudoaneurysms with stent-graft: Analysis of immediate and long-term results. Cir Esp 2017;95:283–92.
Crossref| PubMed - Cochennec F, Riga CV, Allaire E et al. Contemporary management of splanchnic and renal artery aneurysms: results of endovascular compared with open surgery from two European vascular centers. J Vasc Endovasc Surg 2011;42:340–6.
Crossref| PubMed - Kok HK, Asadi H, Sheehan M et al. Systematic review and single-center experience for endovascular management of visceral and renal artery aneurysms. J Vasc Interv Radiol 2016;27:1630–41.
Crossref| PubMed - Parmar H, Shah J, Shah B, et al. Imaging findings in a giant hepatic artery aneurysm. J Postgrad Med 2000;46;104–5. PMID: 11013477″ target=”_blank”>PubMed
- Akbulut S, Otan E. Management of giant splenic artery aneurysm. Medicine (Baltimore) 2015;94:e1016.
Crossref| PubMed - Long CD, Bakshi KR, Kahn MB, Roberts AB. Giant splenic artery aneurysm. Ann Vasc Surg 1993;7:474–8.
Crossref| PubMed - Pescarus R, Montreuil B, Bendavid Y. Giant splenic artery aneurysms: case report and review of the literature. J Vasc Surg 2005;42:344–7.
Crossref| PubMed - Graham LM, Stanley JC, Whitehouse WM Jr, et al. Celiac artery aneurysms: historic (1745–1949) versus contemporary (1950–1984) differences in etiology and clinical importance. J Vasc Surg 1985;2:757–64.
Crossref| PubMed - D’Ayala M, Deitch JS, deGraft-Johnson J, et al. Giant celiac artery aneurysm with associated visceral occlusive disease. Vascular 2004;12:390–3.
Crossref| PubMed - Rodrıguez-Caulo EA, Araji O, Miranda N, et al. Fusiform giant splenic artery aneurysm. Cir Esp 2014;92:215–6 [in Spanish].
Crossref| PubMed - Tiberio GA, Bonardelli S, Gheza F, et al. Prospective randomized comparison of open versus laparoscopic management of splenic artery aneurysms: a 10-year study. Surg Endosc 2012.
Crossref| PubMed - Barbaros U, Ozemir IA, Aksakal N, et al. Laparoscopic surgery of the splenic artery and vein aneurysm with spontaneous arteriovenous fistula. Surg Laparosc Endosc Percutan Tech 2013;23:e127–30.
Crossref| PubMed - O’Driscoll D, Olliff SP, Olliff JF. Hepatic artery aneurysm. Br J Radiol 1999;72:1018–1025.
Crossref| PubMed - Miao YD, Ye B. Intragastric rupture of splenic artery aneurysms: three case reports and literature review. Pak J Med Sci 2013;29: 656–9.
Crossref| PubMed - Al-Habbal Y, Christophi C, Muralidharan V. Aneurysms of the splenic artery: a review. Surgeon 2010;8:223–31.
Crossref| PubMed - Rehman ZU. Multiple giant splenic artery aneurysms with hypersplenism and portal hypertension: a case report. Ann Vasc Dis 2019;12:250–2.
Crossref| PubMed - Rossi M, Virgilio E, Laurino F, et al. Giant hepatic artery aneurysm associated with immunoglobulin g4-related disease successfully treated using a liquid embolic agent. Korean J Radiol 2015;16: 953–4.
Crossref| PubMed - Nguyen AT, Jensen RJ, Lindegaard Pedersen B. Gigantic ruptured aneurysm of the gastroduodenal artery successfully treated by coiling. EJVES Short Rep 2019;45:10–13.
Crossref| PubMed - Abdallah FF, Serracino-Inglott F, Ananthakrishnan G. Giant hepatic aneurysm presenting with hematemesis successfully treated with an endovascular technique. Vasc Endovasc Surg 2017;51:331–4.
Crossref| PubMed - Zhang W, Fu YF, Wei PL, et al. endovascular repair of celiac artery aneurysm with the use of stent grafts. J Vasc Interv Radiol 2016;27:514–8.
Crossref| PubMed - Gjoreski A, Risteski F, Damjanoski G. successful endovascular treatment of a giant hepatic artery aneurysm with dual layer stents placement as flow-diverting option: case report. Open Access Maced J Med Sci 2019;7:403–6.
Crossref| PubMed - Spiliopoulos S, Sabharwal T, Karnabatidis D, et al. endovascular treatment of visceral aneurysms and pseudoaneurysms: long-term outcomes from a multicenter European study. Cardiovasc Intervent Radiol 2012;35:1315–25.
Crossref| PubMed - Hamid HKS, Suliman AEA, Piffaretti G, et al. A systematic review on clinical features and management of true giant splenic artery aneurysms. J Vasc Surg 2019;71:1036–45.e1.
Crossref| PubMed - Xiao N, Mansukhani N, Resnick S, Eskandari M. Giant celiac artery aneurysm. J Vasc Surg Cases Innov Tech 2019;5:447–51.
Crossref| PubMed - Yasumoto T, Osuga K, Yamamoto H, et al. Long-term outcomes of coil packing for visceral aneurysms: correlation between packing density and incidence of coil compaction or recanalization. J Vasc Interv Radiol 2013;24:1798–1807.
Crossref| PubMed - Pitton MB, Dappa E, Jungmann F, et al. Visceral artery aneurysms: Incidence, management, and outcome analysis in a tertiary care center over one decade. Eur Radiol 2015;25:2004–14.
Crossref| PubMed